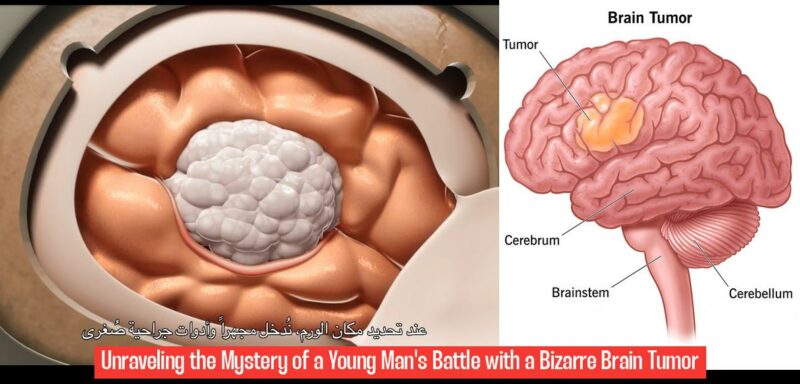
How a Weird Cancer Hit One Young Man Inside the Head

A Nightmare Battle with a Rare Brain Tumor Mirrors a Disturbing Trend
It started with a headache. Nick Fields was on a work-related Zoom call when, mid-sentence, he saw the whites of his eyes suddenly turn bloodshot red. The accompanying pain struck like a lightning bolt – his head, he thought, was splitting open. He quickly turned off his camera before falling to his knees and vomiting. “I need a minute,” he choked out.
That was on March 7. At that moment, his random, painful headache was just that: a random, painful headache. However, before the week was out, the 30-year-old UC Santa Barbara grad and longtime local would find out that “bad headache” was actually a brain tumor the size of a golf ball, and not just any brain tumor, but one that would stump pathologists for months before they could accurately diagnose it.
But while his case turned out to be an anomaly, it fits in with a strange uptick of weird and rare cancers noticed across the country since the beginning of the pandemic. This unsettling trend raises questions about whether the COVID-19 virus could be playing a role in the emergence of these unusual cancers.
Nick’s story is a stark reminder that even the seemingly healthy can be struck by unexpected and devastating illnesses. His journey highlights the importance of seeking medical attention for seemingly minor symptoms, as well as the challenges of navigating a complex and sometimes unpredictable healthcare system.
The story also highlights the importance of community support during times of adversity. Nick’s friends, family, and colleagues rallied around him, providing emotional support, practical assistance, and financial resources as he battled his illness.
The case of Nick Fields is a compelling example of how a seemingly ordinary headache can turn into a life-altering diagnosis. His journey serves as a cautionary tale, prompting us to be more aware of our own health and the potential impact of seemingly minor symptoms.
Why Not Me?
“It felt like somebody hit me over the head with a baseball bat,” Nick told me in April. “I never felt that pain in my entire life,” he said, recounting the day the headache struck. We were talking over coffee at Dune on State Street – well, actually, he was drinking tea, as coffee is generally not recommended for people recovering from brain surgery. Half his head was shaved, showing a new, question-mark-shaped scar.
With a striking lightheartedness, Nick shared the terrifying series of events that followed that mysterious migraine. I had to fight back tears as this otherwise healthy young man told me his story without any perceptible anger or frustration. He was alone in Mammoth Lakes, renovating the condo he and his girlfriend recently purchased, when he developed a severe migraine. Initially, he thought it was altitude sickness, and he drove home to Santa Barbara – a “wild mistake,” he would later call it – but the headache persisted no matter how much caffeine or Tylenol he consumed.
After failing to sleep it off at home, he went to urgent care, where he told them that he had altitude sickness. They treated him but said to come back if the pain persisted. Over the next two days, the migraine only got worse. He got a CT scan.
Within 24 hours, Nick had a neurosurgeon, underwent an emergency brain operation, and had the entire tumor removed. “It all happened very quickly,” he said. But what Nick and his doctors did not know was what to diagnose the tumor.
It was a hypochondriac’s worst nightmare: A severe headache turns into an aggressive brain tumor — an extremely rare, hard-to-diagnose tumor. “The fact that I’m 30 years old and in good health gives me the best chance,” he said. “But it’s a really depressing thing to be told at 30 years old that your time is limited.” Doctors couldn’t tell him if he would ever again be able to work at his company, Santa Barbara–based startup Product Plan, or enjoy his normal life, surfing and playing drums in his tight-knit bands: Uncle Uncle and Pookie.
“A lot of people have said to me, ‘It’s so not fair’ [and] ‘Why you?’ ” he recalled. “But I don’t think life is fair. I don’t think there’s a rulebook. My mantra has been, ‘Why not me?’ I’m better equipped to handle this than someone else. I’ve got a wonderful support system. … So, why not me?” he asked.
“I’m treating it as a chance to really look at life differently. I’m not happy about it. But I have to find the silver linings where they are.”
An Absolute Mouthful
A tissue sample was sent to pathology labs to determine the type of cancer. But the tumor was so rare that doctors struggled to categorize it; even after a month, all they could tell him was that it was a “high-grade glioma,” a very aggressive form of brain cancer. “The typical outlook for someone with a high-grade glioma is usually short, but for me, it’s all unknown,” he said. “You don’t want to be that person. You want to be the one that fits neatly into a box that they know exactly how to treat.”
While the sample was being passed around among multiple pathologists trying to determine a diagnosis, Nick was starting chemotherapy and radiation. His doctors wanted to be “as aggressive as they could” to give him his best shot at remission. He was nauseated, in pain, and having seizures as a residual symptom of the tumor. He felt helpless.
“You can imagine the world of thoughts, emotions, and questions I was in,” Nick said. And on top of that, he was recovering from brain surgery, which is no picnic. He had to relearn to walk and to do the simplest tasks. “Your emotional regulation is out of whack from the surgery,” he added. “And there’s just so many things that are strange.” Uncertainty dominated his life. He was waiting for a diagnosis that seemed more and more terrifying every day.
“It stumped us,” said Nick’s Cottage Hospital nurse navigator Chelsea Brooks. “So, we sent it to a more specialized center. And it stumped them.”
Eventually, the data ended up in Maryland, in the hands of the National Institute of Health. Finally, they had an answer. His tumor was an anaplastic pleomorphic xanthoastrocytoma, “and yes, that is an absolute mouthful,” he wrote in an email I received in May.
For the readers not well-versed in medical jargon, this mouthful translates to a high-grade, malignant, extremely rare brain tumor. Fewer than one case per year is reported in the United States. And an effective treatment is not well-understood. To put it bluntly, it is a “you are probably screwed” kind of diagnosis. “We don’t see this type of tumor very often,” explained Brooks, who has been a nurse for more than a decade. “In fact, he’s my first with this type of tumor. Typically, they’re seen more in the pediatric world,” where it more commonly affects teens and children, not men in their thirties. “To see this in someone that’s a bit older has been pretty remarkable,” she noted.
Cancer Gets Weirder

While it has been a waking nightmare, Nick’s case is not as surprising as it might have been a few years ago, pre-pandemic. Ever since COVID-19 battered the world, there has been an international rise in unusual cancers, a phenomenon discussed in a Washington Post article this June.
To explore how Nick’s case might match these other weird cancers, I called up Dr. Kashyap Patel, a past president of the Community Oncology Alliance, a national group of independent cancer specialists. He and others in his field hosted a symposium about a year ago, exploring this rise in unusual cancers.
The increase in aggressive, late-stage cancers since the pandemic began is confirmed by “some early national data and at a number of large cancer institutions,” according to the Post, though “many experts have mostly dismissed the trend as an expected consequence of disruptions to health care that began in 2020.” However, viruses have been believed to cause or accelerate cancer for decades, and some scientists theorize that chronic inflammation resulting from the COVID-19 virus could exacerbate the growth of cancer cells.
Patel, who works as an oncologist at the Carolina Blood and Cancer Care Associates in Rock Hill, South Carolina, also thinks the effects of COVID-19 could be cumulative in people infected multiple times. Pandemic-related stress may also worsen inflammation, adding to the risk.
“As an oncologist, I’ve known that about, I would say, one in five cancers in the U.S. is linked to some sort of viral infection,” Patel explained. “So, there are trends noticed in the past with cancers. The thing that’s most worrisome is virtually every human being on Earth has had the COVID-19 virus.”
Others are skeptical, though, and suggest the rise in unusual cancers could potentially be due to other toxic stressors, such as tobacco, alcohol, asbestos, or microplastics. Nonetheless, multiple medical institutions – including UC San Diego Health – have compiled data showing an increase in late-stage cancers since the pandemic.
Patel was first struck by this harrowing trend at a weekly lunch with oncologist colleagues in 2021. He was noticing rare and aggressive cancers in patients, and in patients younger than he normally would have seen. Patel was explaining how he had a 40-year-old patient with a rare, lethal bile duct cancer that typically affects people around 65 to 70 years of age. He was surprised to learn that his colleagues had also been seeing similar cases. By the end of the year, his office alone had recorded seven such cases.
During our conversation, Patel noted the main trends he has observed: young patients with very rare cancers, a few patients with multiple new cancers in the two years post-COVID, a few couples with new and rare cancers, and higher numbers of new, rare cancer cases year after year since 2020. They have also seen 30-40 patients have multiple cancers, back-to-back.
“I interact regularly with my international colleagues in India who have seen similar trends,” Patel added. “These are trends I have not seen in my 25 years of being an oncologist.” The most common primary form of brain cancers in adults are called glioblastomas. Before the pandemic, Patel would see maybe one case every five years. Now, it’s more like “three, four, or five” glioblastomas every year.
There’s no question that Nick’s case meets the criteria for “weird”: He has no known family history or genetic predisposition, his cancer is extremely rare, and he is out of the usual age range for patients. Nick also has had COVID twice – once, he was “quite sick” for a time in 2021 – but it cannot be known whether Nick’s case is at all connected to this trend, or to coronavirus, or just an extremely unfortunate coincidence. However, it is interesting how much is unknown, he said.
“Being so rare, I’ve had a weird amount of attention from doctors,” Nick wrote me in an email. “Researchers from UCSF, Mayo Clinic, Johns Hopkins, etc. have looked at it, but probably just as much because they want to collect data as they want to help treat it, which is good, but also scary.”
When talking to Patel about Nick’s experience, he kept coming back to one of his patients, Bonnie Kroll, who had neither a family history of cancer nor a predisposition. She had three biopsies before they could diagnose her cancer. It progressed so rapidly that by the time of the fourth biopsy, it was the size of a football. Patel had never seen her type of aggressive sarcoma in his whole career, but “here she is, growing one in front of me in a matter of weeks,” Patel said.
However, Patel stressed that there is no real-world data linking SARS-CoV-2 to cancer, nor have there been studies to link the coronavirus vaccine and cancer. “But, overall, this is something that we need to study in more detail; we are preparing some prospective research on it. We cannot fathom the depth of what we are dealing with.”
Since the Washington Post article came out, several people who are not his patients have reached out to Patel. So far, he has collected data from more than 35 patients that have been diagnosed with rare cancers since the pandemic began in 2020. He is preparing a database linking Long COVID markers and unusual cancers, to be published before the end of the year.
Patel, however, is concerned about the potential impact of this information going to the general public, “because it’s going to, in my opinion, create some sort of paralysis of normalcy, because when too many people get these chronic illnesses that we don’t understand, it definitely can cause society to kind of pause a little bit.”
No doubt Nick’s life has been put on pause by his unexpected cancer. “Certainly scary,” Nick wrote to me about his diagnosis, “and we’re preparing for another six months of chemo, but holding onto hope that it means we still got a chance here.”
Embracing the Unknown
Chelsea Brooks works with patients at Cottage, like Nick, who would otherwise be left “trying to figure out the fragmented health system on their own.” In Brooks’s words, Nick has “embraced the unknown” and worked with the little information they had to dive headfirst into treatment. “I think that that takes a lot of bravery and trust in a community that he didn’t know existed, right?”
“It’s so easy with this type of diagnosis to turn over and bury your head in the sand,” she continued. “Nick has not,” despite the 20-40 hours of doctor’s appointments he has gone through basically every week since he was first diagnosed. It is, essentially, a full-time job.
Nick’s care team at Cottage’s Ridley-Tree Cancer Center frequently meets with outside experts in rare tumors, collaborating, providing ideas, and comparing notes to make informed decisions for Nick’s treatment. Because his tumor is so rare, they have had to meet more frequently than usual, especially as more information trickled in about his diagnosis.
There was a lot of waiting to determine the next steps for his treatment. However, they have been able to customize his treatment and establish a kind of toolkit in case he has a recurrence. So far, that has not happened.
“My job is a horrible way to meet the most amazing people,” Brooks smiled. “If anyone deserves to have their moment to shine, and be an inspiration for others going through similar situations, it’s Nick. He’s a glowing light — I tell my other patients, ‘If he can do it, you can too.’ ”
Not Saying ‘Uncle’
With support from the people around him, Nick said he feels like he can explore every treatment option, without having to limit himself. His girlfriend’s sister, who works in healthcare, set up his GoFundMe, and his friend Haley Sorensen created a “Meal Train” for people to sign up and bring him food during the first month of his treatment. Not to mention his girlfriend, Rebecca Fox, who has taken time off of work to help him through all the doctor’s appointments, tests, and treatment.
Each friend I spoke to called Nick a “special guy,” someone they said has lived his life with enthusiasm and kindness – even when he worked at Jersey Mike’s in Isla Vista, he was a “passionate sub-making machine.” There are some in his life who have experienced the pain and uncertainty of cancer. They have reached out, helping him to “feel optimistic, and not think about those dark places that your mind can go.”
Nick’s story is a reminder of the resilience of the human spirit. Even in the face of a challenging diagnosis and uncertain future, he has found the strength to embrace the unknown and to continue to live his life to the fullest. His journey is a testament to the power of community support, the importance of hope, and the indomitable spirit that resides within us.
What were the initial symptoms that Nick Fields experienced before his diagnosis?
Nick Fields initially experienced a sudden and severe headache, accompanied by bloodshot red eyes, causing him to fall to his knees and vomit during a work-related Zoom call.
What was the diagnosis for Nick Fields’ symptoms?
The “bad headache” that Nick Fields experienced was diagnosed as a brain tumor the size of a golf ball, which proved to be a rare and challenging case for pathologists to accurately identify.
What trend in cancer cases does Nick Fields’ story align with?
Nick Fields’ case aligns with a disturbing trend of weird and rare cancers that have been noticed across the country since the beginning of the pandemic, raising questions about the potential role of the COVID-19 virus in the emergence of these unusual cancers.
How did Nick Fields’ community support him during his battle with cancer?
Nick Fields received emotional support, practical assistance, and financial resources from his friends, family, and colleagues as he navigated his illness, highlighting the importance of community support during times of adversity.